- Patients & Visitors
- Patient Information
- Insurance & Billing Information

Insurance & Billing Information
For more billing information, the following pages are available for you to read.
- Frequently Asked Questions
- Preguntas Frecuentes
- Business Office
- Discount Program (please call the Business Office)
- Debt Collection Practices
We want to make it as simple as possible for you to manage the costs of services. By discussing the expenses in advance with your doctor, your insurer and the hospital, you will be better able to manage and understand your medical bills.
Our Business Office will bill your primary insurance company, one secondary insurance company and any third-party insurance company. Even if Marshall bills your insurance, you remain responsible for payment for all care you receive. This may include care denied or not covered by your insurance, as well as your deductible and copayment amounts.
In addition to your hospital bill, you may receive separate bills from physicians involved in your care, such as your primary care physician, radiologist, emergency services physicians, surgeons, anesthesiologists, and other consulting physicians. Please contact these services directly with any billing questions.
No Surprises Act
Effective January 1, 2022, the No Surprises Act, which Congress passed as part of the Consolidated Appropriations Act of 2021, is designed to protect patients from surprise bills for emergency services at out-of-network facilities or for out-of-network providers at in-network facilities, holding them liable only for in-network cost-sharing amounts. The No Surprises Act also enables uninsured patients to receive a good faith estimate of the cost of care.
Billing Disclosures – Your Rights and Protections Against Surprise Medical Bills
When you get emergency care or get treated by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from surprise billing or balance billing.
What is “balance billing” (sometimes called “surprise billing”)?
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, such as a copayment, coinsurance, and/or a deductible. You may have other costs or have to pay the entire bill if you see a provider or visit a health care facility that isn’t in your health plan’s network.
“Out-of-network” describes providers and facilities that haven’t signed a contract with your health plan. Out-of-network providers may be permitted to bill you for the difference between what your plan agreed to pay and the full amount charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same service and might not count toward your annual out-of-pocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care–like when you have an emergency or when you schedule a visit at an in-network facility but are unexpectedly treated by an out-of-network provider.
You are protected from balance billing for:
Emergency services
If you have an emergency medical condition and get emergency services from an out-of-network provider or facility, the most the provider or facility may bill you is your plan’s in-network cost-sharing amount (such as copayments and coinsurance). You can’t be balance billed for these emergency services. This includes services you may get after you’re in stable condition, unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services.
Additionally, California law protects patients with coverage through plans regulated by the California Department of Managed Care from balance billing when the patient receives emergency services from an out-of-network doctor or hospital. This protection only requires patients to pay their in-network cost sharing amounts.
Certain services at an in-network hospital or ambulatory surgical
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers may bill you is your plan’s in-network cost-sharing amount. This applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can’t balance bill you and may not ask you to give up your protections not to be balance billed.
If you get other services at these in-network facilities, out-of-network providers can’t balance bill you, unless you give written consent and give up your protections.
You’re never required to give up your protections from balance billing. You also aren’t required to get care out-of-network. You can choose a provider or facility in your plan’s network.
Additionally, California law protects patients with health care service plans from balance billing when patients receive covered services at an in-network facility by an out-of-network provider. This protection requires patients to only pay their in-network cost-sharing amount. If the patient consents to services in advance, the balance billing prohibition does not apply.
When balance billing isn’t allowed, you also have the following protections:
- You are only responsible for paying your share of the cost (like the copayments, coinsurance, and deductibles that you would pay if the provider or facility was in-network). Your health plan will pay out-of-network providers and facilities directly.
- Your health plan generally must:
- Cover emergency services without requiring you to get approval for services in advance (prior authorization).
- Cover emergency services by out-of-network providers.
- Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility and show that amount in your explanation of benefits.
- Count any amount you pay for emergency services or out-of-network services toward your deductible and out-of-pocket limit.
If you believe you’ve been wrongly billed, you may contact:
- The U.S. Centers for Medicare & Medicaid Services (CMS) at 1-800-MEDICARE (1-800-633-4227) or visit https://www.cms.gov/nosurprises for more information about your rights under federal law.
- The California Department of Managed Health Care at 1-888-466-2219 or visit https://www.dmhc.ca.gov/ for more information about your rights under California law.
- The California Department of Insurance at 1-800-927-4357 or visit https://www.insurance.ca.gov/01-consumers/110-health/60-resources/NoSupriseBills.cfm for more information about your rights under California law.
If you do not know what kind of plan you have, you can call the California Department of Insurance Help Center at 1-800-927-4357.
Good Faith Estimate
You have the right to receive a “Good Faith Estimate” explaining how much your medical care will cost.
Under the law, healthcare providers need to give patients who don’t have insurance or who are not using insurance an estimate of the bill for medical items and services.
- You have the right to receive a Good Faith Estimate for the total expected cost of any non-emergency items or services. This includes related costs like medical tests, prescription drugs, equipment and hospital fees.
- Make sure your healthcare provider gives you a Good Faith Estimate in writing at least one business day before your medical service or item. You can also ask your healthcare provider, and any other provider you choose, for a Good Faith Estimate before you schedule an item or service.
- If you receive a bill that is at least $400 more than your Good Faith Estimate, you can dispute the bill.
- Make sure to save a copy or picture of your Good Faith Estimate.
Get More Information
For questions or more information about your right to a Good Faith Estimate, visit cms.gov/nosurprises or call 1-800-MEDICARE (1-800-633-4227).
Notice to patients: Open payments database
A link to the federal Centers for Medicare and Medicaid Services (CMS) Open Payments web page is provided for informational purposes only. The federal Physician Payments Sunshine Act requires that detailed information about payment and other payments of value worth over ten dollars ($10) from manufacturers of drugs, medical devices, and biologics to physicians and teaching hospitals be made available to the public.
Search the federal database for payments made to physicians and teaching hospitals
Price Transparency - Health Care Charges
We know how it is important for you to understand your healthcare options and costs. To ensure price transparency as required by Federal regulations, we are providing our fee listings for each of our service areas.
Insurance companies negotiate contracted amounts with hospitals and medical groups. This contracted amount often reduces the fee that is used to calculate your out-of-pocket expenses. Marshall’s contracted amount (and therefore the amount Marshall receives from the various companies/Medicare/Medi-Cal) is on average substantially less than the charges that are included in the documents provided below.
Additionally, as a non-profit entity, some of the payments we receive do not cover the costs of providing care. We make every effort to balance out all payments we receive to ensure we can continue to provide quality care to our community and maintain our operations. Marshall offers many charity care and financial assistance policies to patients who are uninsured or underinsured and require financial assistance based on their income.
Marshall accepts a wide array of health insurance plans and it is important that you verify that Marshall Hospital and/or specialty is included in your health plan’s network of contracted hospitals and physicians to assist in limiting your out-of-pocket costs.
Important Note:
The fees provided below do not take into account your insurance benefits or the amount that Marshall has agreed to under any insurance plan (i.e., employer benefit, Medicare or Medi-Cal). Please contact your insurance company for a pre-treatment estimate/pre-treatment authorization which is designed to provide you with a more comprehensive explanation of your potential out-of-pocket costs.
- Hospital Services - PDF
- Hospital Services - Machine Readable
- Clinic Services - PDF
- Clinic Services - Machine Readable
- Pharmacy Services - PDF
- Pharmacy Services - Machine Readable
- Surgical Supply Services - PDF
- Surgical Supply Services - Machine Readable
- Average hospital charges by standard diagnosis groupings (MS-DRG) - PDF
- Average hospital charges by standard diagnosis groupings (MS-DRG) - Machine Readable
- Marshall Standard Charges
For Marshall Employees
The regulations for Consolidated Appropriations Act (CAA), the No Surprises Act (NSA), and Transparency in Coverage are designed to provide greater consumer protections for Marshall employees and their families. As part of this legislation, group health plans and insurers are required to provide machine-readable files (MRF) disclosing information about costs, covered items, and their services. This information is available for Marshall's Third Party Administrator, Health Comp, on this website: https://healthcomp.sapphiremrfhub.com/
For assistance with your hospital bill or to request an itemized statement, please call our business office at 530-626-2618 or email hpcbilling@marshallmedical.org.
Related Blogs
-
 For Your Health, Spring 2025
For Your Health, Spring 2025- Newsletter
Read More -
 For Your Health Spring 2022
For Your Health Spring 2022- Newsletter
Click here to read the latest issue of For Your Health.
Read More -
 For Your Health, Fall 2024
For Your Health, Fall 2024- Marshall In The News
Marshall For Your Health – Fall 2024
Read More -
 Marshall Nationally Recognized for Exceptional Care
Marshall Nationally Recognized for Exceptional Care- Press Release
Read More -
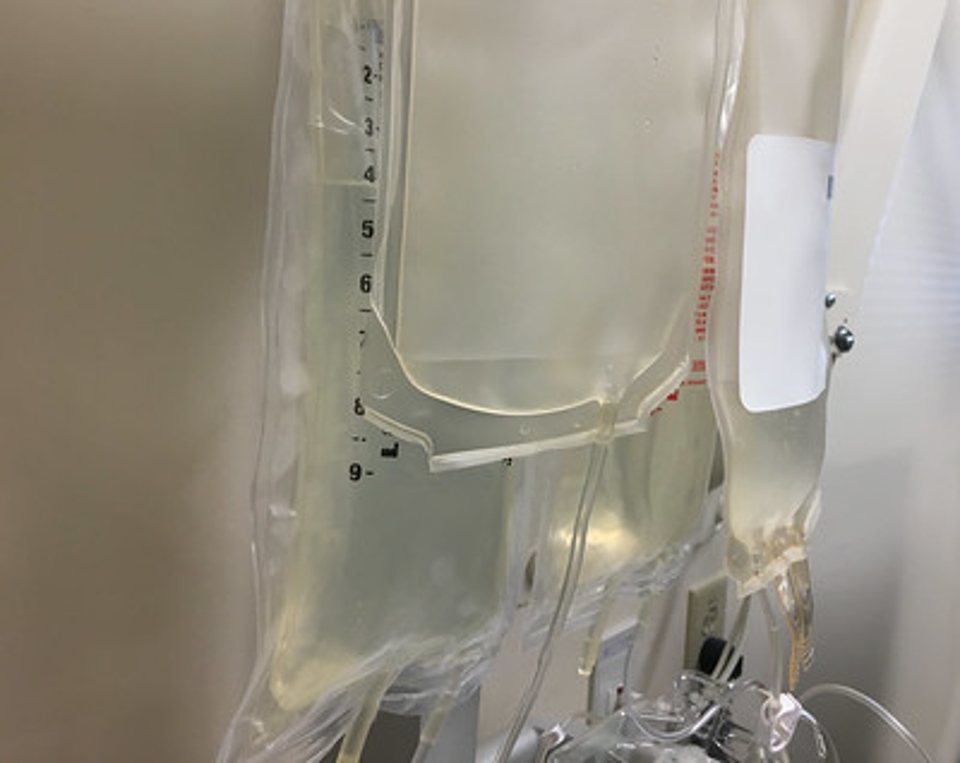 Marshall Takes Proactive Measures to Respond to National IV Fluid Shortfall
Marshall Takes Proactive Measures to Respond to National IV Fluid Shortfall- Press Release
As has been reported in the national media, Hurricane Helene severely damaged one of the major suppliers of intravenous (IV) fluids used to care for ...
Read More -
 Marshall Named Top Hospital in Patient Safety and Quality Care
Marshall Named Top Hospital in Patient Safety and Quality Care- Marshall In The News
- Press Release
Digital platform Money, in partnership with national watchdog organization The Leapfrog Group, has named Marshall one of 148 top hospitals in the ...
Read More -
 Why Do I Still Have to Wear a Mask in a Hospital?
Why Do I Still Have to Wear a Mask in a Hospital?- Ask the Expert
Just about everywhere you go these days, indoor mask mandates for public spaces have been dropped. In communities like El Dorado County with low rates ...
Read More -
 Marshall Affiliates with UC Davis Health for World-Class Cancer Care
Marshall Affiliates with UC Davis Health for World-Class Cancer Care- Marshall In The News
- Press Release
Marshall and UC Davis Health have announced an affiliation for cancer services that allows Marshall patients access to the renowned UC Davis ...
Read More -
 For Your Health, Fall 2023
For Your Health, Fall 2023- Marshall In The News
Download the PDF here
Read More -
 Self-Schedule on MyChart
Self-Schedule on MyChart- Press Release
Your convenience is our priority. Log in to your MyChart account and schedule or cancel many types of appointments with ease, with the family and ...
Read More


